The Sprint 8 exercise protocol is a novel
approach to fighting obesity efficiently among middle-aged
females by substantially increasing GH serum levels naturally
--------------------------------------------------------------------------------
David Braden, MD1,2; JRoss, MD1; LC Gray, MD 1;
C Walker, RN, MSN1; A Hoover, MS, MEd1; and S Duane Burt,
MS1,3
1 King's Daughters Medical Center, Brookhaven, MS, USA
2 University of Mississippi Medical Center, Jackson, MS,
USA
3 Copiah-Lincoln Community College, Wesson, MS, USA
--------------------------------------------------------------------------------
Corresponding Author: S Duane Burt, Science Department,
Copiah-Lincoln Community College, 1028 JC Redd Dr., Wesson,
MS, 39191, USA. Email: duane.burt@colin.edu Phone: (601)
643-8369 June 2, 2012
Funding: This research received no specific grant from
any funding agency in the public, commercial, or not-for-profit
sectors. This study was conducted at and funded by King's
Daughters Medical Center (KDMC), Brookhaven, MS, USA.
ABSTRACT
Background: The Sprint 8 exercise protocol
described in Ready, Set, Go! Synergy Fitness for Time-Crunched
Adults [7] has shown to fight obesity economically and time-efficiently
by naturally invoking significant growth hormone (GH) release.
GH serum levels are known to increase substantially after
exercise, where it initiates lipolysis, inhibits the uptake
and storage of other lipids, and induces muscle hypertrophy.
Objectives: The goal of this novel approach to fighting
obesity was to efficiently maximize natural GH release among
middle-aged African-American and Caucasian females [mean
age = 45.9 (±7.7 yrs)] to metabolize adipose tissue
and reduce hyperlipidemia by utilizing the Sprint 8 protocol.
By documenting pre- and post-trial GH and lipid serum values,
body fat %, and BMI, the correlated health benefits produced
by each subgroup were established for future studies.
Method: This 8-week, free-living, Sprint
8 trial required 8 hours of exercise (20 min, 3 days/week),
without dieting. The protocol intermittently incorporates
intermediate fast-twitch (type IIA) and fast-twitch (type
IIB) muscle fibers with their associated aerobic and anaerobic
metabolic processes, substantially increasing body temperature
and lactic acid production, which lowers blood pH, affording
significant GH release.
Results: Among 22 participants, GH serum values increased
603% following the initial bout and 426% final bout. Post-Sprint
8 trial afforded reductions in body fat (-27.4%), BMI (-3.9%),
cholesterol (-9.6%), LDLs (-12.4%), triglycerides (-16.1%),
and HDLs increased 2.0%.
Conclusions: The Sprint 8 shows to
be a natural, economical, and efficacious obesity-reduction
strategy among middle-aged females. These individuals benefit
socially and physically, while healthcare systems benefit
financially.
INTRODUCTION AND BACKGROUND
Obesity
It is well documented that obesity is a major problem in
the U.S. and other countries. It is associated with many
diseases, disabilities, discriminations, and financial hardships.[1]
Obesity is correlated with hyperlipidemia or elevated blood
cholesterol, LDL, and triglycerides, accompanied with low
HDL serum levels.[2] Hyperlipidemia leads to many cardiovascular
diseases (CVDs), particularly atherosclerosis, which is
the leading cause of death for men and women not only in
the U.S., but in the world.[3,4] Additionally, the healthcare
industry is burdened with the billions of dollars spent
on the many ensuing chronic diseases derived from the over-shadowing
obesity epidemic. Some of the diseases and problems evolving
from obesity include: hyperlipidemia, diabetes, hypertension,
coronary heart disease, osteoarthritis, gall bladder disease,
impaired fertility, complications during pregnancy, breathlessness,
sleep apnea, gout, low-back pain, and cancer. Indeed, the
highest utilization costs in the healthcare industry belong
to CVDs. [5,6] In order to reduce patient suffering, as
well as alleviating the financial burden carried by the
healthcare industry, the need for an efficacious intervention
is crucial.
Indeed, these health complications and financial
burdens derived from obesity plague the U.S., where Mississippi
is consistently ranked as the most obese state. King's Daughters
Medical Center (KDMC) in Brookhaven, MS has an interest
in fighting obesity in our state and beyond by employing
the Sprint 8 exercise protocol, as described in the book,
Ready, Set, Go! Synergy Fitness for Time-Crunched Adults
[7]. The Sprint 8 protocol shows here to be time-saving,
financially efficient, and extremely effective at naturally
inducing the release of growth hormone (GH) in significant
amounts, which is known to be a major factor in triggering
lipolysis.
Exercise and Growth Hormone
While obesity is the root of innumerable complications,
exercise defends the body against just as many impediments.
Furthermore, exercise as a drug of choice for personal health
and wellness is monetarily free. It is also well documented
that any exercise regimen is a major component to having
a healthy lifestyle, and that growth hormone (GH) release
and exercise are correlated. The National Institutes of
Health reports that exercise-induced GH, when released,
can increase up to 500% and stay significantly elevated
beyond two hours.[8] During this time, GH is known to have
multiple functions and produce numerous benefits, including
playing a role in muscle hypertrophy and targeting the metabolism
of triglycerides, the foundation of not only obesity and
hyperlipidemia, but the other ensuing diseases previously
noted.[9,10] It is generally accepted that anaerobic exercise
shows to increase GH levels far more than aerobic activities
alone; [10,11] however, research is scarce when studying
intermediate fast-twitch (type IIA) and fast-twitch (type
IIB) muscle fibers with their associated anaerobic metabolic
processes and the resulting effect of GH release during
exercise. What is understood is that when undertaking anaerobic
activity, such as sprinting, lactic acid builds in the muscular
system and ultimately the blood, where blood pH is lowered.
Body temperature is also dramatically elevated during anaerobic
exercise. Increased body temperature and the declining pH
of blood induces GH release from the anterior pituitary
gland, possibly for the purpose of repairing muscles by
way of elevating amino acid uptake within muscle cells,
increasing muscle cell protein synthesis, [12] and also
increasing sweat release to cool the body.[13] In turn,
increased GH values trigger insulin-like growth factor 1
(IGF-1) release from the liver, as well as from other tissues,
including muscle tissue. IGF-1 is known to be a potent anabolic
hormone. GH and IGF-1 synergistically increase muscle cell
protein synthesis leading to muscle hypertrophy. [14,15]
At the same time, GH initiates lipolysis within adipose
tissue for energy. Adipose cell membranes contain GH-binding
protein receptors. When binding to adipose receptors, GH
stimulates the metabolism of triglycerides while inhibiting
the uptake and accumulation of other circulating lipids.[16]
Therefore, when utilizing types IIA and IIB muscle fibers
intermittently during exercise (sprints), exceptionally
high GH serum levels are produced, which direct the building
of muscle mass that ultimately feeds on adipose for maintenance
and increases the metabolic rate of fatty tissue. It is
apparent that obesity is attacked far more efficiently than
with the utilization of type I muscle fiber alone and that
elevated exercise-induced GH serum levels show to have promising
effects for the growing problem of obesity and associated
hyperlipidemia.
However, most popular anti-obesity programs
today only utilize slow-twitch (type I) muscle fibers, which
include mostly aerobic physiological processes, such as
walking, jogging, or the like. These programs do not take
advantage of the surplus of GH that could be produced by
incorporating type IIA and IIB muscle fibers, such as intermittent
sprints, or other intensive bursts of activity. Furthermore,
these popular programs focus on a calories-in, calories-out
diet, accompanied with other lifestyle changes, and the
recommended time necessary (30 minutes per exercise, 5 days
a week) on the exercise component is daunting, while results
are slow to develop. These low intensity and lengthy aerobic
exercises, coupled with a strict diet, tend to reduce participant
adherence to a program, and therefore often fail. [7, 17]
The Sprint 8 Protocol
The underlying thesis behind the Sprint 8 protocol is to
optimally and efficiently maximize exercise-induced GH release
by exercising under intermittent anaerobic conditions to
intentionally and substantially elevate body temperature
and induce lactic acid accumulation to subsequently reduce
body fat. [7] As previously described, both of these processes
are known to naturally induce the anterior pituitary gland
to release significant quantities of GH into blood serum
where it initiates lipolysis. Along with the common utilization
of type I muscle fibers, the Sprint 8 intermittently incorporates
types IIA and IIB muscle fibers, engaging anaerobic metabolism
to continue muscle function. This produces large amounts
of lactic acid and increases body temperature substantially,
which stimulates GH release from the anterior pituitary
gland into blood serum, where it then initiates adipose
lipolysis and promotes muscle cell anabolism. [12,13] The
abundant release of GH produced by the Sprint 8 regimen
promotes major fitness-improving benefits, as well as time-saving
benefits in regard to exercise, that are realistic and achievable
by most healthy adolescents and adults. The Sprint 8 requires
20 minutes per bout, 3 times per week, totaling 8 hours
of exercise per 8 weeks. Additionally, there is no diet
required, and the muscular system benefits. The Sprint 8
exercise protocol was developed by a healthcare professional
who is a certified trainer with the American College of
Sports Medicine with 37 years of experience. It was created
in the 1990s and is published in the 384-page book entitled
Ready, Set, Go! Synergy Fitness for Time-Crunched Adults,
by Campbell, (2001, 2010).[7] The protocol is consistent
with the latest cardiovascular guidelines (2007) established
by the American Heart Association and the American College
of Sports Medicine for vigorous intensity cardiovascular
exercise. [7] In this novel approach to finding relief for
the obesity crisis, preliminary studies of the Sprint 8
protocol indicate that GH is released naturally and abundantly
during the program and produces a wealth of promising data
in dealing with not only reducing body fat and increasing
muscle mass, but with the obesity and hyperlipidemia epidemic.
MATERIALS AND METHODS
Subjects (Pre-Sprint 8 trial)
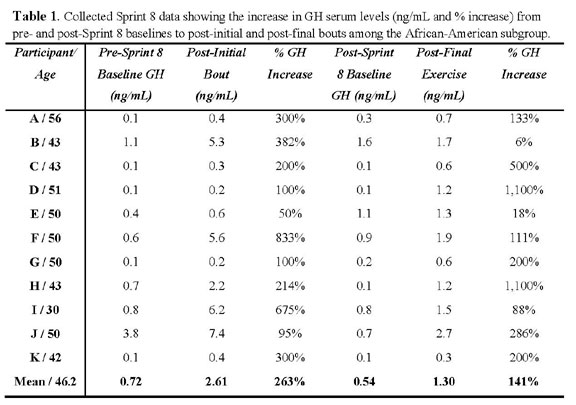
Twenty-two (22) females, aged 30-57 [mean age (±SD)]
= 45.9 (±7.7 yrs.), mean mass 97.3 kg (214 ±48.2
lbs.), mean body fat % = 40.2 (±7.2%), mean BMI =
36.0 (±7.6 kg/m2), mean GH baseline level = 0.94
(±1.2 ng/mL), mean blood cholesterol level = 207.6
(±39.8 mg/dL), mean blood LDL level 136.8 (±35.5
mg/dL), mean blood triglyceride level = 93.0 (±54.4
mg/dL), mean blood HDL level = 51.5 (±9.6 mg/dL),
participated in this eight-week, free-living, Sprint 8 trial.
The 22 participants were composed of eleven (11) African-American
females, mean age = 46.2 (±6.9 yrs), mean mass 106
kg (233 ±49.0 lbs.), mean body fat % = 43.1 (±6.2%),
mean BMI = 39.5 (±6.9 kg/m2), mean GH baseline value
= 0.72 (±1.1 ng/mL), mean blood cholesterol level
= 196.8 (±31.6 mg/dL), mean blood LDL level 130.0
(±27.2 mg/dL), mean blood triglyceride level = 77.8
(±37.1 mg/dL), mean blood HDL level = 51.0 (±10.1
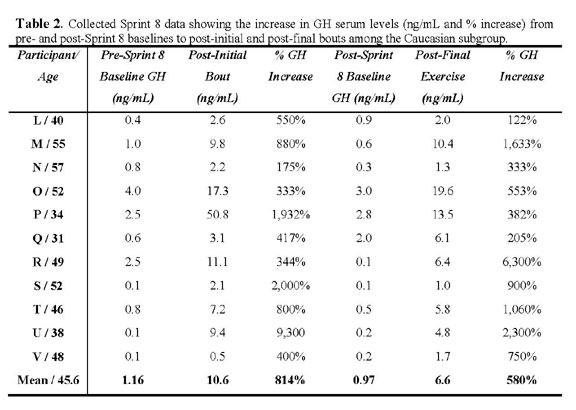
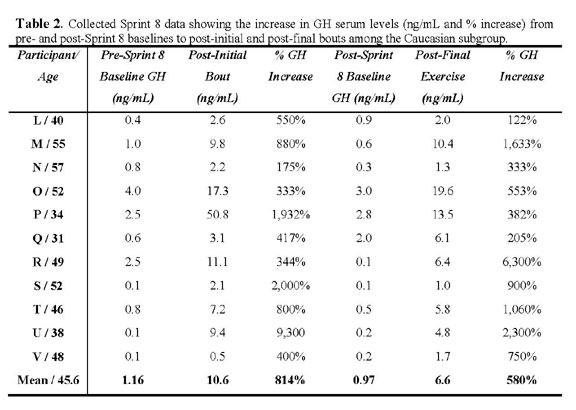
mg/dL); and eleven (11) Caucasian females, mean age = 45.6
(±8.7 yrs), mean mass 87.9 kg (194 ±40.0 lbs.),
mean body fat % = 37.0 (±7.1%), mean BMI = 32.6 (±6.9
kg/m2), mean GH baseline value = 1.16 (±1.1 ng/mL),
mean blood cholesterol level = 218.3 (±45.6 mg/dL),
mean blood LDL level 143.6 (±42.5 mg/dL), mean blood
triglyceride level = 113.4 (±61.7 mg/dL), mean blood
HDL level = 52.0 (±9.5 mg/dL).
Before the initial blood work and first Sprint 8 bout, a
KDMC, Sprint 8-certified trainer held a 45 minute preparatory
session with all participants to explain the physiological
concepts and protocol of the Sprint 8 program, as outlined
in Campbell's book entitled Ready, Set, Go! Synergy Fitness
for Time-Crunched Adults [7]. This project was free-living,
where participants received no KDMC oversight during the
8 week program, as to represent a realistic setting, and
their project adherence was strictly voluntary. Participants
were asked to continue their usual, daily routines, with
no dietary or prescribed medication changes. During this
eight week trial, the only variable on health measures was
the impact of the Sprint 8 protocol.
Sprint 8 Trial
The Sprint 8 trial (2012) was conducted over an eight-week
period, three Sprint 8 bouts per week, 20 minutes per bout,
totaling 8 hours of exercise during the 8-week trial period,
and with no specific diet. Participants were free to choose
among stationary-upright or recumbent bikes, treadmills,
and/or elliptical trainers as their exercise equipment at
any given session. Individual Sprint 8 bouts were held at
KDMC's Fitness Center, Brookhaven, MS. In any given bout,
participants began with a 2.5 minute warm-up period, also
known as the "active recovery pace" (ARP), followed
by 30 seconds of full-sprint cardiovascular activity to
increase body temperature and induce anaerobic metabolism
with associated lactic acid build-up and elevated body temperature.
Because fitness levels are different among participants,
when gauging a "sprint" vs. an ARP, the sprint
component should maintain a minimum of 40 RPMs higher than
the ARP for the duration of the 30 second sprint. After
the initial 30 second sprint component, subjects returned
to their ARP for 1.5 minutes. After the 1.5 minute ARP,
subjects repeated the sprint component for 30 seconds. This
process continued until eight sprints were performed, with
a final 3 minute cool-down period, totaling 20 minutes per
bout.
Blood Sampling and Analysis
A panel of lab tests indicative of health and wellness were
conducted pre- and post-Sprint 8 trial for baseline measurements.
Cholesterol, triglyceride, LDL, HDL, and GH serum levels
were obtained from each participant to determine the impact
of the program on basic health and wellness. Blood lipids
(cholesterol, triglycerides, LDL, and HDL) were analyzed
by a Siemens Dade Dimension® ExL™ integrated chemistry
system at King's Daughters Medical Center, Brookhaven, MS.
GH level assays were performed by Laboratory Corporation
of America® Reference Laboratory (LabCorp) in Birmingham,
AL, which analyzes GH by the immunochemiluminometric (ICMA)
assay method. Initial 10 hour fasting blood tests were conducted
pre-Sprint 8 trial to establish a baseline measurement.
A total of 16.0 mL of whole blood was drawn from each subject,
with 4.0 mL of plasma used for the basic metabolic and lipid
panel measures, 5.0 mL of ethylenediaminetetraacetic acid
(EDTA) plasma used to test glycated hemoglobin (A1C) levels,
and 2.5 mL of serum sent to LabCorp for GH measure. Additionally,
7.0 mL of blood was drawn within 30 minutes of the initial
bout of the Sprint 8 program with 2.5 mL of serum sent to
LabCorp for another GH post-exercise measure. Final blood
labs identical to those measured in week one were performed
at the end of week eight, both fasting for a post-trial
baseline, and within 30 minutes of the final bout of the
program for a final GH measure.
Weight, Body Fat %, and BMI
Weight, body fat percentage, and BMI data were obtained
pre- and post-Sprint 8. Weight measurements were obtained
utilizing a Rice Lake® medical scale. Body fat percentage
results were obtained by employing a Futrex-5000Ai®
body fat analyzer which uses IR light refraction. The measurements
were taken on the dominate bicep of test subjects. BMI measurements
were acquired using the Body Mass Index Calculator of the
U.S. Department of Health and Human Services National Heart,
Lung, and Blood Institute. These measurements were obtained
from participants pre- and post-Sprint 8 trial.
RESULTS
GH Values
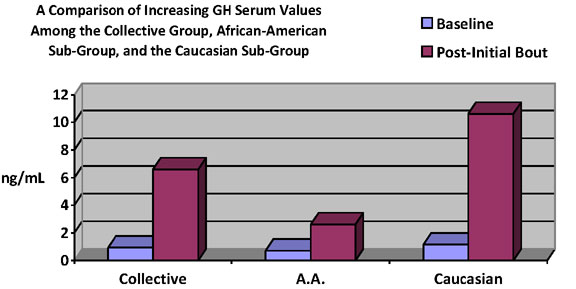
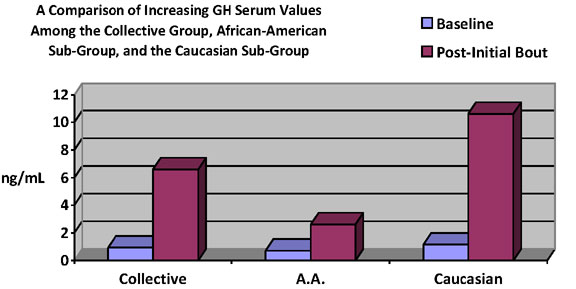
The collective mean GH serum value of the 22 participants
was 6.6 (±10.8 ng/mL) and was obtained within 30
minutes of finishing the initial bout, day 1. Here, GH levels
increased 603% from the collective pre-trial baseline value
(0.94 ng/mL). Additionally, the collective mean baseline
GH serum level obtained pre-exercise, post-Sprint 8 trial
was 0.76 (±0.86 ng/mL). When compared to 4.0 (±4.8
ng/mL), the collective mean GH serum level taken within
30 minutes of the post-final bout, post-Sprint 8 trial,
the data affords a 426% increase of GH serum levels.
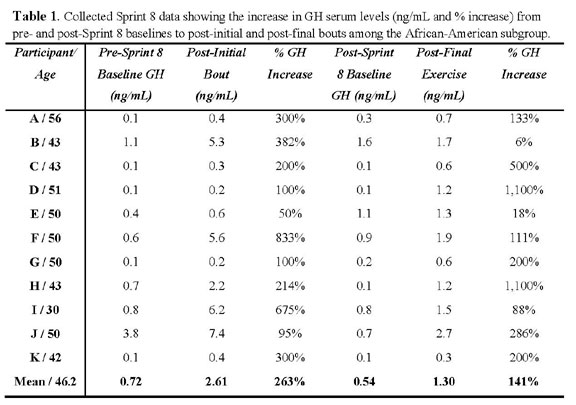
When observing the African-American group, the initial-bout
GH serum value increased 263% from the pre-trial baseline
value (0.72 ±1.0 ng/mL), where the African-American
collective mean was 2.61 (±2.9 ng/mL), post-initial
bout. The collective African-American post-trial, post-final
exercise GH level was 1.3 (±0.7 ng/mL) and elevated
141% when compared to the collective mean baseline obtained
pre-exercise, post-trial (0.54 ±0.51 ng/mL).
The Caucasian group increased GH serum values 814% during
the initial bout, where the collective Caucasian mean GH
serum level was 10.6 (±14.3 ng/mL) post-initial bout,
increasing from the pre-trial baseline value of 1.16 (±1.3
ng/mL). The post-trial baseline GH value was 0.97 (±1.0
ng/mL) and increased 580%, where the post-trial, final-bout
GH value was 6.6 (±5.8 ng/mL). Collective, African-American
subgroup, and Caucasian subgroup comparisons of GH serum
values pre-Sprint 8 baselines to post-initial Sprint 8 bouts
are represented in Graph 1. Subgroup and individual GH data
are presented in Table 1 and Table 2.
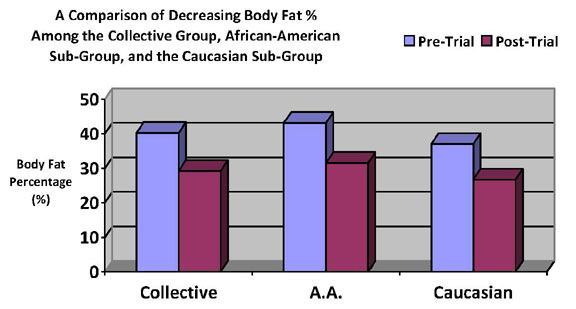
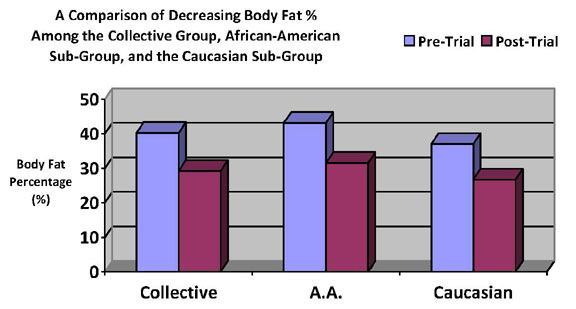
Body Mass (Post-Sprint 8 trial)
The 22 participants collectively lost 67.3 kg (148 lbs.)
of adipose tissue. On average, each subject lost 3.0 kg
(6.8 lbs.) of fatty tissue. Post-trial mean body mass =
93.6 kg (206 ±48.2 lbs.). Post-trial mean body fat
% = 29.2 (±5.3%), where mean body fat % reduction
= 27.4%. Post-trial mean BMI = 34.6 (±7.7 kg/m2),
and post-trial mean BMI reduction percentage = 3.9%.
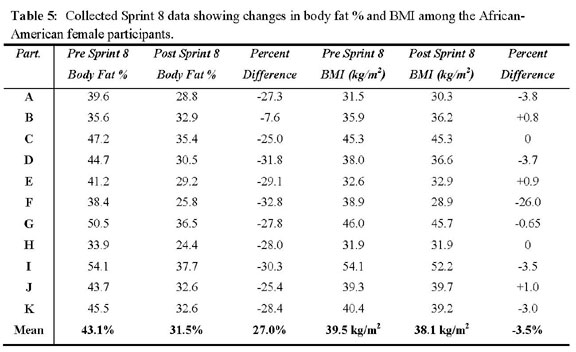
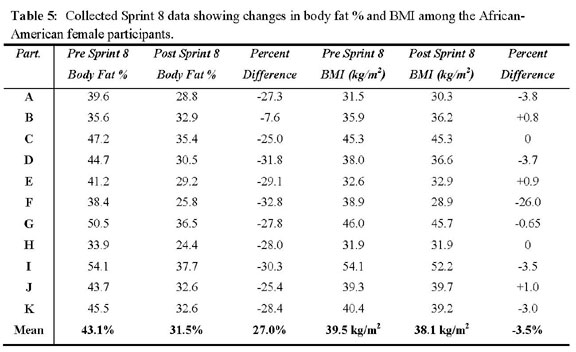
The African-American group collectively metabolized 24.5
kg (54 lbs.) of adipose tissue. On average, each subject
lost 2.23 kg (4.9 lbs.) of fatty tissue. The post-trial
mean mass = 103.5 kg (228.4 ±48.1 lbs.). Post-trial
mean body fat % = 31.5 (±4.2%), mean body fat % reduction
= 27.0%, post-trial BMI = 38.1 (±7.3 kg/m2), post-trial
mean BMI percentage reduction = 3.5%.
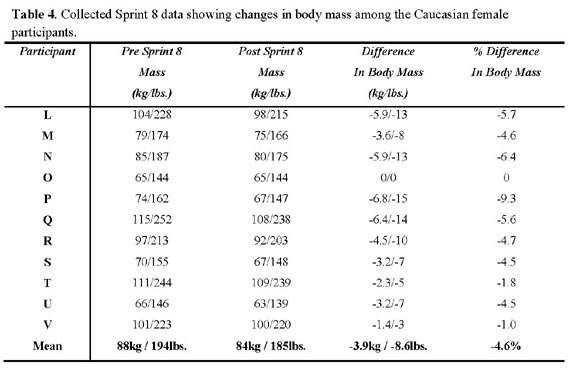
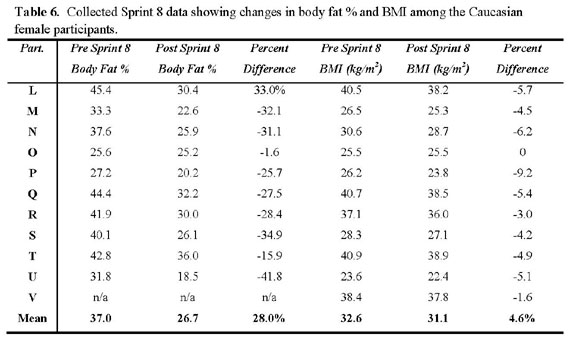
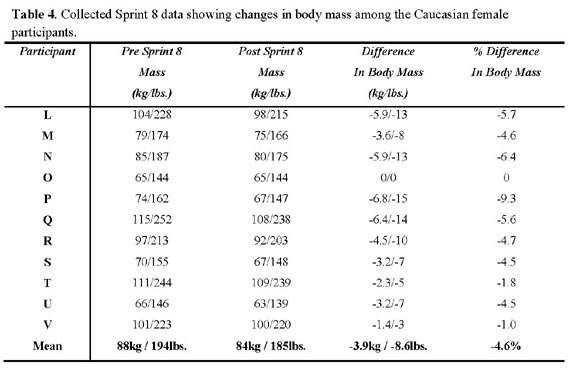
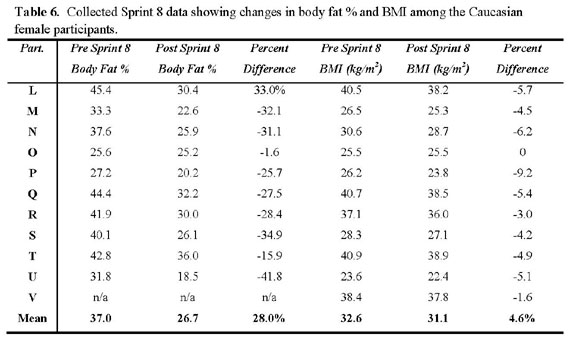
The Caucasian group collectively metabolized 42.7 kg (94
lbs.) of adipose tissue. On average, each subject lost 3.88
kg (8.5 lbs.) of fatty tissue. The post-trial mean mass
= 84.0 kg (184.9 ±39.0 lbs.). Post-trial mean body
fat % = 26.7 (±5.5%), mean body fat % reduction =
28.0%, post-trial BMI = 31.1 (±6.7 kg/m2), post-trial
mean BMI percentage reduction = 4.6%. Individual and subgroup
body mass data are represented in Table 3, Table 4, Table
5, and Table 6. Body fat percentage reductions are depicted
in Graph 2.
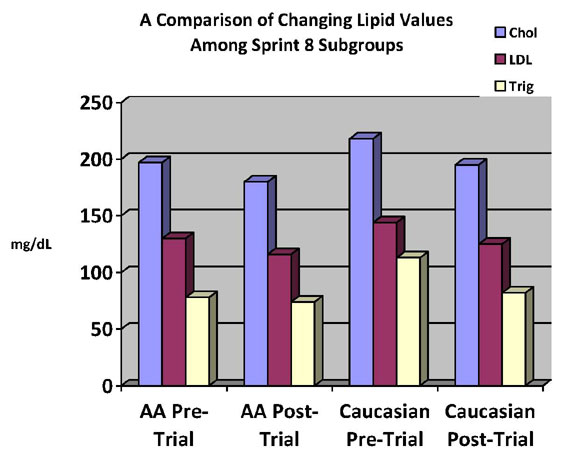
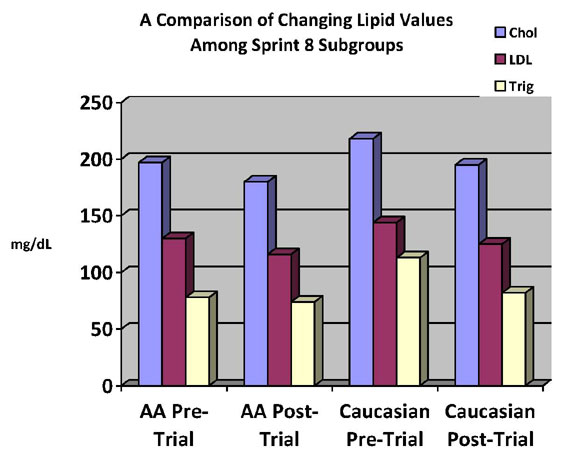
Lipid Levels (Post-Sprint 8 trial)
Collective mean cholesterol serum level = 187.8 (±30.9
mg/dL), mean blood cholesterol % loss = 9.6%, mean blood
LDL level = 120.5 (±28.6 mg/dL), mean blood LDL %
loss = 12.4%, mean blood triglyceride level = 93.0 (±54.4
mg/dL), mean blood triglyceride % loss = 16.1%, mean blood
HDL level = 52.0 (±9.9 mg/dL), mean HDL % increase
= 2.0%.
The African-American subgroup cholesterol serum value =
180.3 (±24.3 mg/dL), mean blood cholesterol % loss
= 8.4%, mean blood LDL level = 115.9 (±20.7 mg/dL),
mean blood LDL % loss = 10.9%, mean blood triglyceride level
= 74.5 (±38.1 mg/dL), mean blood triglyceride % loss
= 4.3%, mean blood HDL level = 49.5 (±8.9 mg/dL),
mean HDL % decrease = 2.9%.
The Caucasian subgroup cholesterol serum value
= 195.4 (±35.9 mg/dL), mean blood cholesterol % loss
= 10.5%, mean blood LDL level = 125.1 (±35.2 mg/dL),
mean blood LDL % loss = 13.2%, mean blood triglyceride level
= 82.3 (±26.4 mg/dL), mean blood triglyceride % loss
= 27.4%, mean blood HDL level = 54.6 (±10.7 mg/dL),
mean HDL % increase = 5.8%. Table 7 and Table 8 identify
lipid value data. Graph 3 exhibits the changes of these
lipid serum values in mg/dL among the African-American and
Caucasian female subgroups, pre- and post-Sprint 8 trial.
DISCUSSION AND CONCLUSIONS
In this realistic-representative, free-living
study with no specific diet, where Sprint 8 adherence was
entirely voluntary, the 22 participants produced a collective
body fat reduction of 27.4%, a BMI decrease of 3.9%, and
metabolized 67.3 kg (148 lbs.) of adipose tissue, all within
8 hours of exercise during the 8-week trial. Among the African-American
and Caucasian subgroups, body fat % reductions were remarkably
similar, within 1.0% difference. The African-American subgroup
pre-trial BMI value was substantially higher than the Caucasian
subgroup pre-trial BMI value and appears not to have diminished
as significantly as the Caucasian subgroup post-trial. However,
that knowledge itself indicates that the declining African-American
subgroup post-trial BMI value is as equally impressive as
the Caucasian subgroup post-trial BMI value. BMI and body
fat percentage of all African-American participants were
found to be at unhealthy ranges pre-Sprint 8 trial. Furthermore,
this is where their greatest results were produced, with
a 27% reduction in body fat and BMI decreasing 3.5 %.
The collective GH value increased 603% after
the initial bout, and 426% after the final bout of the trial.
The Caucasian subgroup increased GH serum values substantially
more so than the African-American subgroup. A possible explanation
for this lies within the equipment utilized. In this study,
participants were free to choose among stationary upright
bicycles, stationary recumbent bicycles, treadmills, or
elliptical trainers. The African-American subgroup tended
to employ the upright and recumbent bicycles, where the
Caucasian subgroup exploited the elliptical trainers and
treadmills. Compared with the elliptical trainer and treadmill,
the recumbent and upright bicycles show to be the least
intensive of the Sprint 8 equipment options for this study,
where no substantial upper-body activity assists during
any given bout with the utilization of the bicycles. This
could explain the reduced GH serum values presented with
the African-American subgroup because body temperature and
lactic acid production would be somewhat diminished without
major upper body involvement. This possibly leads to an
entirely separate study involving the psychology associated
with how individuals wish to exercise, and perhaps their
adherence to any given exercise program.
For both subgroups, the changes in serum lipid
values were surprisingly unexpected, where the Sprint 8
protocol appears to mimic cholesterol-lowering medications.
This demands further investigation. As previously discussed,
this free-living study required participants to adhere to
their daily lives as usual, including no changes in diet
or prescribed medications. A number of the Sprint 8 test
subjects described after the brief 8 week trial that they
no longer required various medications that they were previously
prescribed, most of which were high blood pressure or cholesterol-reducing
medications. While not all participants were at risk for
CVDs, cholesterol lowered 9.6%, LDL dropped 12.4%, triglycerides
decreased 16.1%, while HDLs increased 2.0%, all within 8
weeks. Although body fat percentage and BMI values of the
African-American subgroup were initially unsuitable, serum
lipid values were in healthy ranges pre-trial. However,
with the utilization of the least-intensive Sprint 8 equipment,
this subgroup decreased its serum lipid value further into
the healthy range, indicating the efficacy of the Sprint
8 protocol.
It is well known that GH has been touted as a miracle drug
and an anti-aging medication. It has been banned from organized
competitive athletics due to the anabolic effects and resulting
unfair advantages it produces. Because of the many other
positive physiological effects GH is known to produce, billions
of dollars are spent annually on artificial and supplemental
GH therapy, both legally and illegally. However, side effects
are associated with artificial GH injections, and they include:
hyperlipidemia, arthritis, cardiomegaly, impotence, weakened
glucose regulation and possibly type 1 diabetes. Research
indicates that exercise-induced GH release is natural, more
potent, and much safer than artificial injections.[10,16,18]
However, past research has acknowledged the beneficial results
exercise-induced GH produces and has proposed that finding
the optimal factors in obtaining the greatest natural GH
release remains elusive. These Sprint 8 trial results indicate
that exceptionally high amounts of exercise-induced GH are
released during this exercise protocol, and these elevated
GH levels show to combat obesity. Due to the lack of research
involving types IIA and IIB muscle fibers coupled with GH
release during exercise, more studies are necessary regarding
the Sprint 8. For example, studies involving other specific
population groups, with a primary focus on childhood obesity;
changes that may occur in naturally GH deficient patients;
the health-related effects produced among participants undertaking
long-term Sprint 8 activity; the Sprint 8 program linked
with a diet; strength training with naturally elevated GH
levels; the effects to those who have high blood pressure
and/or taking prescribed cholesterol-lowering medications;
participants with various hormonal imbalances, such as dysfunctional
thyroid glands, declining testosterone levels, or depression;
among others.
In a quest to fight obesity and all of these
underlying problems within our state and beyond, King's
Daughters Medical Center (KDMC) has a significant interest
in exploring and utilizing the natural production of exercise-induced
growth hormone (GH) in this contest. By tracking GH blood
serum levels and corresponding changes in body fat percentage,
BMI, and lipid values, and other measures as warranted,
KDMC wishes to continue studying the health benefits produced
by the Sprint 8 program on these various populations.
The Sprint 8 program is a novel approach to
potentially fighting the obesity epidemic and the many health
and financial problems stemming from it. Beyond improving
patient health, the Sprint 8 program has the potential to
relieve the burden placed on the health care industry by
the innumerable diseases and disabilities derived from obesity
and hyperlipidemia. Billions of dollars could be saved in
health care expenses. As an alternative to the popular aerobic
activities that require 30 minutes of exercise 5 days per
week to be minimally effective and coupled with diets that
depend on counting calories, the Sprint 8 proves to be time-efficient,
at 20 minutes per bout, 3 bouts per week, for 8 weeks, totaling
a mere 8 hours of exercise per 8 weeks, and requires no
specific diet due to the significant amounts of GH the program
yields. Building from this trial, as well as from future
findings, an entire better way of life can be found for
so many, categorized as obese or not.
ACKNOWLEDGEMENTS
King's Daughters Medical Center (KDMC) is
grateful for the participation and endurance of the volunteers
who participated in this study. A special thank you is necessary
for Mr. Alvin Hoover, CEO, KDMC, and Mr. Phil Campbell,
COO, KDMC, for supporting the study. Elizabeth Smith was
responsible for much of the organization, data collection,
and oversight of the project, and we are gratified with
her work. Additionally, we are thankful for Todd Peavey,
KDMC Fitness Center Manager, and the KDMC Fitness Center
staff who provided knowledge, support, and encouragement
for the volunteers. Emma Coleman, KDMC Lab Manager, and
her staff are greatly appreciated for performing the appropriate
blood work. Finally, we thank all of the physicians and
other medical staff at KDMC for their support in KDMC taking
the initiative to find a solution to the obesity epidemic.
DECLARATION OF CONFLICTING INTERESTS
The authors declare that there is no conflict of interest.
FUNDING
This research received no specific grant from
any funding agency in the public, commercial, or not-for-profit
sectors.
REFERENCES
1. Ehrman JK, Gordon PM, Visich PS, and Keteyian
SJ (Editors). Clinical Exercise Physiology, Second Edition.
Human Kinetics Publishing, Champaign, IL, 2009.
2. Curran, MP. 2010. Amlodipine/Atorvastatin,
a Review of its Use in the Treatment of Hypertension and
Dyslipidaemia and the Prevention of Cardiovascular Disease.
Drugs, 70 (2), pp. 191-213.
3. Loyd-Jones D, Adams R, Carnethon M, et
al. 2009. Heart disease and stroke statistics - 2009 update:
a report from the American Heart Association Statistics
Committee and Stroke Statistics Subcommittee. Circulation,
119 (3), pp. 21-181.
4. World Health Organization (WHO). 2009.
"World Health Report 2009", pp. 144-145, 150-151.
5. Thom T, Haase N, Rosamond W, et al. 2006.
Heart Disease and Stroke Statistics - 2006 update: a report
from the American Heart Association Statistics Committee
and Stroke Statistics Subcommittee. Circulation, 113, pp.
85-151.
6. Dragomir A, Cote R, White M, Lalonde L,
Blais L, Berard A, and Perreault S. 2010. Relationship between
Adherence Level to Statins, Clinical Issues and Health-Care
Costs in Real-Life Clinical Setting. Value in Health, 13
(1), pp. 87-94.
7. Campbell, P. Ready, Set, GO! Synergy Fitness
for Time-Crunched Adults, 2nd Edition. Pristine Publishers,
Nashville, TN, 2010.
8. Stokes KA, Nevill NE, Hall GM, and Lakomy
HK. 2002. The time course of the human growth hormone response
to a 6 s and a 30 s cycle ergometer sprint. J Sports Sci,
20 (6), pp. 487-494.
9. Gilbert KL, Stokes KA, Hall GM, and Thompson
D. 2008. Growth hormone responses to 3 different exercise
bouts in 18- to 25- and 40- to 50-year-old men. App. Physiol.
Nutr. Metab., 33, pp. 706-712.
10. Kanaley, JA. 2008. Growth hormone, arginine
and exercise. Curr Opin Nutr Metab Care, 11, pp. 50-54.
11. Kon M, Ikeda T, Homma T, Akimoto T, Suzuki
Y, and Kawahara T. 2010. Effects of Acute Hypoxia on Metabolic
and Hormonal Responses to Resistance Exercise. Med Sci Sports
Exerc., 42 (7), pp. 1279-1285.
12. Fryburg DA, Gelfand RA, and Barrett EJ.
1991. Growth hormone acutely stimulates forearm muscle protein
synthesis in normal humans. Am J Physiol, 260, pp. 499-504.
13. Jorgensen JO, Krag M, Kanaley J, Hansen TK, Moller N,
Christiansen JS, and Orskov H. 2003. Exercise, hormones,
and body temperature regulation and action of GH during
exercise. J Endocrinol Invest., 26 (9), pp. 838-842.
14. Kozlowski S, Chwalbinska-Moneta J, Vigas
M, et al. Greater serum GH response to arm than leg exercise
performed at equivalent oxygen uptake. Eur J Appl Physiol,
52, pp. 131-135.
15. Florini JR, Ewton DZ, and Coolican SA.
1996. Growth hormone and the insulin-like growth factor
system in myogenesis. Endocr Rev. 17, pp. 481-517.
16. Godfrey RJ, Madgwick Z, and Whyte GP.
2003. The Exercise-Induced Growth Hormone Response in Athletes.
Sports Med, 33 (8), pp. 599-613.
17. Trapp EG, Chisholm DJ, Freund J, and Boutcher
SH. 2008. The effects of high-intensity intermittent exercise
training on fat loss and fasting insulin levels of young
women. Int J Obesity, 307, pp. 1-8.
18. Kicman AT and Cowan DA. 1992. Peptide
hormones and sport: misuse and detection. Br Med Bull, 48,
pp. 496-517.
TABLES AND GRAPHS
Graph 1. Results of the Sprint 8 showing the
increase in GH serum values (ng/mL) when comparing pre-Sprint
8 trial baseline and post-initial bout. Depicted are the
participants collectively, the African-American subgroup,
and the Caucasian subgroup, where GH values increased 603%,
263%, and 814%, respectively.
Graph 2. Results of the Sprint 8 showing the
decrease in body fat % when comparing pre-Sprint 8 trial
baseline body fat percentages and and post- 8 week trial
baseline body fat percentages. Depicted are the participants
collectively, the African-American subgroup, and the Caucasian
subgroup, where body fat percentages decreased 27.4%, 27.0%,
and 28.0%, respectively.
Graph 3. Results of the Sprint 8 trial, comparing
points (mg/dL) of cholesterol, LDL, and triglycerides, pre-Sprint
8 (baseline) and post-Sprint 8, among the African-American
and Caucasian female subgroups.

How to do Sprint 8 Cardio here
Diseases Attributed to Obesity here